Fun Fact: October was Ultrasound Awareness Month!
I cannot tell you how bummed I am to learn that there is a whole month dedicated to educating about/celebrating what I do, yet that month has come and gone!
I feel like it might be a little late now to do a full-on celebration, but in the spirit of spreading awareness about the job I love, I thought I would share with you some of the anomalies I have found in my career in perinatology thus far.
For those who aren’t aware, I work as a sonographer in a perinatology department, which means that I do ultrasounds on high-risk mothers and/or mothers with high-risk pregnancies.
Having done this for years now, I have seen a variety of abnormalities that presented themselves in utero (which means while the baby is still in the uterus).
These abnormalities have not only improved my abilities and skillset as a sonographer, but also in being an empathetic human being.
Through ultrasound, sonographers and other healthcare providers alike, are able to bring a unique form of clarity and peace when anomalies are found. Not only are we able to prepare beforehand for the special needs of mother and child when the baby is born, but we are also able to bring knowledge and comfort in a way that no one else in a patient’s support system can. In having seen similar cases and being educated on stats, studies, and causes, we are able to provide insight based on the aforementioned. In most cases, these abnormalities catch the patients and their support system completely off guard, so they feel unable to ask the right questions and helpless towards providing for their child’s newfound needs. The technology of ultrasound, and what it has taught us in the healthcare field, helps us combat that by coming alongside the patient and walking with them step-by-step.
Again, all of the anomalies below are ones I have personally scanned and seen. I am going to include both the more common and well-known anomalies, along with the less. With these, I will include some facts about these anomalies and images showing how they appear on ultrasound. I will link the sources I use, as they are reliable and what the perinatologists I have worked alongside provide patients who have affected babies.
(Also, these images are from Google, so no patient confidentiality has been broken on my part).
(To be considerate, I will include the warning that some of these images may be disturbing or troubling for some readers, so please be both respectful of those who have had these anomalies appear in their own lives and cautious on whether you are comfortable continuing).
1.) Cleft Lip/Palate


Cleft lip is a gap in the upper lip, which can range in severity and where it is located.
On ultrasound, cleft lip is recognized by a notching in lip. While cleft lip can be isolated (the only abnormality the baby has), it can also be associated with micrognathia (a small jaw), cleft palate (a gap in the roof of the mouth), and a flattened face. Extra amniotic fluid around the baby can also be indicative of a cleft lip, due to the baby having difficulty swallowing properly
Due to these other possible abnormalities being present, we sonographers will pay attention to these other areas to rule out whether the baby has a syndrome (multiple abnormalities present) or if the cleft lip is an isolated finding.
2.) Downs Syndrome


Downs Syndrome is a genetic condition that causes developmental and physical delays.
Due to Downs being linked to genetics, it is not diagnosable through ultrasound alone. The only 100% way to determine if the baby is affected while in utero is by an amniocentesis (inserting a needle through the belly, extracting a sample of amniotic fluid, and testing the baby’s genetic material in the fluid).
However, there are soft markers (physical indicatations of a baby possibly being affected) for Downs that can be detected with ultrasound. These include a short/absent nasal bone, a protruding tongue, fluid in the kidneys, etc. These soft markers, if seen, can be relayed to the patient and may give cause for testing, if the patient desires it.
3.) Clubbed Foot


Clubbed foot is a turning of the ankle. One or both feet can be affected.
On ultrasound, clubfoot can be seen and diagnosed through evaluating the angling of the foot. Clubfoot can be either an isolated finding or syndromic. If syndromic, abnormalities such as heart defects (problems with the structure), micrognathia, and clenched fists might be present.
Clubfoot cannot be treated while in utero, but can be once the baby is delivered. Depending on the severity of the clubbing, treatment ranges from braces to surgery.
4.) Ectrodactyly


Ectrodactyly, or Split Hand/Split Foot Malformation, is the clefting of the hands or feet due to the lack of development of the middle fingers/toes.
It can either present unilaterally (one hand/foot affected) or bilaterally (both hands/feet affected). While ectrodactyly can affect both the hands and the feet, it is most popularized as “lobster hands”, associated with 19th-century circus “freak” shows.
On ultrasound, the splitting of the hands and feet can be visualized and diagnosable. While it can be isolated, syndromic indications might include cleft lip/palate and heart defects, so those areas are evaluated as well.
(In the case I scanned, it presented in the hands bilaterally).
5.) Twin-to-Twin Transfusion Syndrome
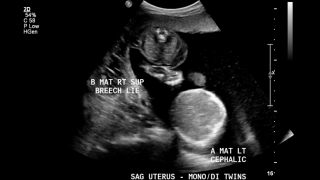
TTTS is a syndrome that can occur in monochorionic-diamniotic twins (each baby has its own sac, but they share the placenta), in which one baby takes blood from the other.
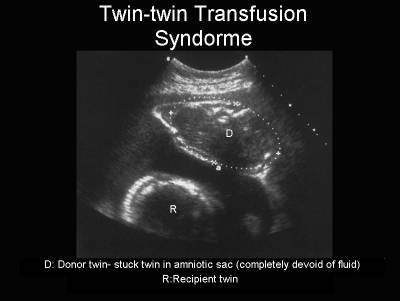
TTTS can be detected and diagnosed through ultrasound. Several indications are used in diagnosing this syndrome, differing between the donor (baby giving blood) and the receipient (baby receiving extra blood).
In the donor baby, symptoms include oligohydramnios (too little/no fluid around baby), little/no urine in the bladder, and small size.
In the receipient baby, symptoms include polyhydramnios (too much fluid around baby), increased amount of urine in the bladder, and large size.
If TTTS is expected, the blood flow in the umbilical cord and brain also can be measured. These measurements can determine if the exchanging of blood is unbalanced, leading to TTTS.
I am so thankful for this career and how it is used to better (even save) lives! I am proud of the work I have done so far and look forward to the work I have yet to do!
It may not be the official awareness month anymore, but thank your local sonographer for all that they do anyways! Sonographers, we salute you!
I am considering making this a series! I’d love to hear your thoughts! Are there any anomalies or syndromes you’d be interested in knowing if/how ultrasound plays a part in diagnosing?